Cervical Cancer facts
Overview
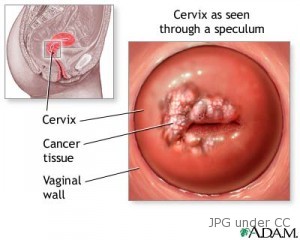
Cervical cancer is a dreadful disease among women where the cells of the cervix start to become abnormal and grow, thus forming tumors. In the U.S., this disease is common among women aged 35-54. It commonly starts in the cells on the outside of the cervix. The cervix is located in the lower part of the uterus, connecting the uterus to the vaginal canal.
Types and forms
About 90% of cervical cancers are squamous cell carcinoma and the 10% are the adenocarcinoma type.
In some occasions, the cervical cancer may have both types and is called adenosquamous carcinoma or mixed carcinoma. The squamous cell carcinomas originate in the thin, flat, squamous (linings) cells on the surface of the part of the cervix next to the vagina (ectocervix), while the adenocarcinoma cancer originates in the mucus-producing cells near the body of the uterus (endocervix).
The initial changes in cervical cell may not be cancerous but lesions (dysplasia) occur within the outer cell layers. These abnormal cells are called cervical intraepithelial neoplasia (CIN).
Carcinoma or non-invasive cervical cancer is the term for moderate to severe dysplasia. Dysplasia is a common condition and disappears even without treatment. However, these can develop into cancer through the years, sometimes even earlier.
Symptoms
Generally, many women do not feel any symptoms for cervical cancer. Symptoms appear only when the disease has already become invasive. Some of these are light vaginal bleeding, abnormal vaginal discharge, pain and bleeding during sexual intercourse, post menopausal bleeding and pains in the pelvic area.
Late stage symptom is heavy vaginal bleeding, fatigue, loss of appetite, leg pain, swollen leg usually single leg only, leaking of the urine or feces from the vagina, bone fractures, weight loss and back pain.
Causes and risk groups
Elderly women are more prone to cervical cancer. Young girls under 15 years of age seldom develop this disease. Risks, however, increase in the late teens. Approximately 90% of all cervical cancers are caused by infection with HPV or human papilloma virus. Some types of HPV are sexually transmitted. Approximately 6 million women in the U.S. are afflicted with HPV infections which have no cure.
Most cervical cancers can be prevented. HPV infection is a very big risk factor especially among young women below 18, whose cells (lining the cervix) are not yet fully mature and are therefore more susceptible to cancer.
HPV, being sexually transmitted, puts many young women with bad sexual behaviors at risk for cervical cancer. Sexual intercourse at a young age, say 16 and below, having multiple sexual partners and having sex with someone who had sex with somebody else afflicted with cervical cancer, are behaviors that may give rise to risks for HPV infections and cervical cancer.
Infection with HIV that causes AIDS is also a cause for cervical cancer. So is the genital herpes virus.
Unhealthy diet, such as that lacking in fruits and vegetables, heightens the risk as well. Other causes are obesity, those whose mothers took the drug diethylstilbestrol (DES), prolonged use of pills and smoking tobacco.
Diagnosis
Cervical cancer used to be a common cause of death but there has been a decrease in mortality rate due to the routine screening with Pap tests or Pap Smear test. This helps identify pre-cancerous and early stages of this disease. Early treatment of these conditions assures almost 100% cure rate. Very often, cervical cancer is first spotted with the Pap Smear Test.
This is part of regular pelvic examination. If the result is positive for abnormalities, treatment is done on the patient. A few months after the treatment of infection, a repetition of the Pap Smear is performed. Biopsies are also done to diagnose this disease. Once diagnosed, the doctor performs a complete physical examination and evaluation of the symptoms.
Treatment
The kind of treatment depends on the stage of the disease. Some treatments to remove precancerous cells or other early-stage cervical cancers include cryosurgery or freezing cells, cauterization or burning off cells and laser surgery which burns off cells via laser beams.
These treatments require close monitoring to detect recurrence of the illness. A simple hysterectomy is performed to remove the uterus, and sometimes the fallopian tubes and ovaries as well.
In a radical hysterectomy, the uterus and adjoining tissues as well as the ovaries, the upper vagina near the cervix and the lymph nodes are all removed. After the hysterectomy, the tissues are examined to verify if cancer has spread to the other parts of the body and whether or not radiation is needed.
If the cancer recurs after treatment, extensive surgery is performed. This surgery includes the removal of the bladder, part of the colon, rectum and/or the entire vagina. A new vagina, though, is created surgically.
Recovery may take some time, two years at the most. If the cancer has spread to other organs, chemotherapy may be used. Chemotherapy kills cancer cells. This treatment is a combination of external and internal radiation and chemotherapy. Chemotherapy has some side effects but these drawbacks are only temporary.
